
How do we move from selective to comprehensive primary health care in low and middle income countries: reflections of an expert panel
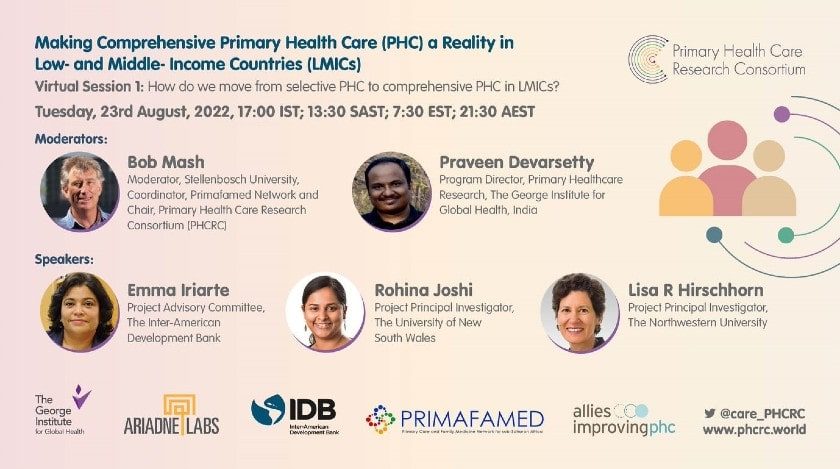
Continuing its advocacy efforts for robust #PrimaryHealthCare and #EvidenceBasedPHC. The Primary Health Care Research Consortium, supported by the PHCPI Micro-Grant for Advocacy, launched its webinar series called ‘Making Comprehensive Primary Health Care a Reality in LMICs’ on 23rd August 2022. Webinar No. 1 targeted the pertinent question, ‘How do we move from selective to comprehensive PHC in LMICs?’, and saw participation from 95 attendees from 40 countries. The panel composed of PHCRC members represented different parts of the globe – South Asia, Asia Pacific, sub-Saharan Africa, and the Americas.
For more updates on the webinar series and PHCRC activities, follow @care_PHCRC
What is the difference between selective and comprehensive PHC?
After the Alma Ata declaration in 1978, which espoused a broad vision of PHC, many countries opted for a more selective approach. They argued that it was more cost-effective to focus on a few priorities and be able to measure progress. Thus, PHC became synonymous with health programmes that focused on specific topics or conditions such as growth monitoring, oral rehydration and diarrhea or later HIV and TB. These programmes typically existed side by side in siloes with their own budgets, management structure, funding and donors. They have been referred to as vertical programmes as they extended throughout the health system from the national level to the PHC facility.
The vision for PHC has always been a more comprehensive one and governments once again committed themselves to this in the Astana Declaration of 2018. The World Health Organization has subsequently described an operational framework for comprehensive PHC that has three key elements (Figure 1). Firstly, multisectoral policy and action to address the social and environmental determinants of health, secondly, empowering communities to address their own health problems and lastly, integrated primary care services with essential public health functions. Governments that implement this would be implementing comprehensive PHC.

Figure 1: The essential elements of comprehensive PHC. Source: WHO
In addition, primary care itself has a number of core functions in order to deliver high quality primary care. These include first contact access, continuity, coordination, person-centredness and comprehensiveness. In this context comprehensive primary care implies services across the life course, for all diseases and conditions, and from health promotion and disease prevention to rehabilitation and palliative care.
Are we still stuck in selective PHC? How big a problem are we tackling?
The focus on vertical programmes for delivering PHC has been seductive and continues in many countries to this day. In reality, this approach has not necessarily been more cost-effective as each programme duplicates the resources needed to run their programme. Programmes are often driven by the availability of donor funds and thus create inequity by disease in the population. For example, a person with HIV may be able to access a well-funded service with many resources in primary care, while a person with diabetes must find help at the hospital level. Vertical disease programmes also fail to address the underlying social and environmental determinants of health such as clean water and sanitation. In addition, PHC staff that work within these siloes are trained to manage only one disease or problem and do not have the ability to function as generalists. Finally, these programmes reduce the ability of PHC to adapt to new challenges and priorities that fall outside the designated focus areas. This results in a health system that lacks responsiveness, adaptability and resilience.
Many countries are beginning to recognize the problems associated with selective PHC, especially with the new call for comprehensiveness in the Astana Declaration. The move towards universal health coverage is also in synergy with a move towards integrating these siloes into a more comprehensive approach to PHC.
What should we do to implement comprehensive PHC?
The panel suggested a number of important actions to help countries move towards more comprehensive PHC:
- The evidence for and examples of comprehensive PHC should be gathered and shared with policymakers
- Countries should have mechanisms for coordinating the use of donor funding and planning together how funds can strengthen comprehensive PHC and not just vertical programmes. Countries should also use their available funds more efficiently to strengthen integrated primary care and comprehensive PHC.
- Countries should re-orientate their PHC workforce away from vertical programmes and selective skills, towards a generalist and comprehensive approach. At the same time we need to ensure a workforce with sufficient numbers and skills mix to avoid burnout and ensure quality. In many countries a PHC team approach includes community health workers, nurses and family doctors.
- Multisectoral policy and action should become a reality and not just an espoused idea in order to tackle the social and environmental determinants of health.
- Community engagement and participation must be prioritized as an essential feature of PHC at the local level.
- Health priorities within a comprehensive approach can be established at the local or sub-national level as well as national.
- Measurement of PHC performance should also be comprehensive. Health systems should measure to take action at the local level and not just to report at the high level.
- There needs to be greater accountability between levels of the health system for progress on comprehensive PHC
- Supervision and management of PHC should shift from a punitive and authoritarian style to a more supportive and collaborative style.
- Countries should establish systems for continuous quality improvement in PHC.
- Economic incentives for the PHC teams may help drive quality improvement.
- Countries need to collaborate and learn from each other on what works to deliver comprehensive PHC.



