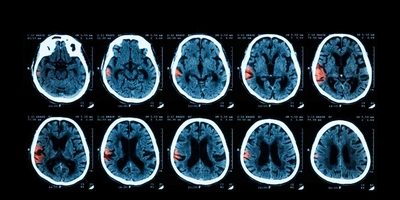
Study confirms benefits of early intensive blood pressure control in acute stroke due to intracerebral haemorrhage
A new study, published in The Lancet Neurology, has revealed an optimal approach to lowering elevated blood pressure (BP) for treating patients with acute stroke due to spontaneous bleeding in the brain (intracerebral haemorrhage or ICH), the most serious type of stroke.
Early and sustained lowering of systolic BP to levels much lower than have previously been considered, less than 130 mmHg (millimetres of mercury), in patients with ICH was shown to provide the best chance of surviving with good recovery from this devastating condition, a new study from The George Institute for Global Health found.
ICH, spontaneous bleeding within the deep or superficial areas of the brain, is most often associated with elevated BP or ‘hypertension’, and affects approximately 2 million people in the world each year, most of whom live in China and other parts of Asia. About one third of those affected die early after onset due to compression of the haemorrhage on vital structures of the brain, and many survivors are left with serious long-term disability.
“There has been controversy from apparent different findings of the two largest trials of rapid BP lowering in ICH - INTERACT2, which I led, and ATACH-II, organised by my United States colleagues. This has caused doubt about the effectiveness of intensive BP lowering as a treatment for acute ICH. So, we joined forces to pool our study data and try and resolve any ongoing uncertainty,” said senior author, Professor Craig Anderson, Executive Director from The George Institute China.
Professor Anderson said the finding from the data pooling project provides strong evidence for the benefits of intensive BP lowering in acute ICH.
The study was a prospective analysis of a total of 3829 patients with ICH and elevated systolic BP who participated in large INTERACT2 and ATACH-II trials investigating intensive BP.
The new pooling project study found significant beneficial associations between early intensive BP reduction and clinical outcomes after ICH, which extends previous analyses, and it identified an optimal systolic BP level of 120-130 mmHg for best recovery, which is lower than previously considered for recommendations in various clinical guidelines around the world.
Key findings:
- Systolic BP is associated with clinical outcomes at 90 days - the lower the achieved mean systolic BP, the more favourable the chances of recovery from ICH. Every 10 mmHg reduction in systolic blood pressure was associated with a 10% increase in the chance of better functional recovery, potentially down to levels of 120-130 mmHg.
- Low fluctuations (or variability) of systolic BP reduce the risk of death and other serious adverse events.
- Lower systolic BP levels are also associated with reduced bleeding in the brain, less neurological deterioration, and better chances of survival free of serious disability.
- However, doctors should be cautious about producing rapid and large drops in systolic BP levels in order to avoid any adverse effects of the treatment.
The study recommended careful reduction to levels less than 130 mmHg over the 24 hour period after the onset of symptoms, and to minimise variability and avoid levels below 120 mmHg, as the optimal approach to early intensive BP control.
“The findings extend current guideline recommendations of controlling systolic BP levels at less than 140 mmHg. Reducing systolic BP to even lower levels provides the best chance of recovery but caution is required at levels below 120 mmHg.”
“We hope the study can help patients with ICH achieve the best recovery with the least risk of adverse events,” said Dr. Xia Wang, Post-Doctoral Research Fellow from The George Institute for Global Health Australia.