Seven George Institute researchers have been announced as recipients of the Government’s 2022 Investigator Grant scheme, designed to support emerging and established leaders in health and medical research across Australia to tackle our greatest health challenges.
The Institute’s successful projects encompass a wide range of these challenges from better ways of treating cardiovascular disease and sepsis, encouraging uptake of salt substitutes, improving the food environment, reducing risks of drowning, and helping Aboriginal and Torres Strait Islander peoples into employment for better health and wellbeing. These are summarised below.
Alta Schutte, Professorial Fellow at The George Institute for Global Health
One third of Australian adults have raised blood pressure, half are unaware of it, and only a third have their blood pressure controlled, leading to preventable strokes, heart attacks and deaths.
Professor Schutte’s research will test four new approaches proven to be effective in other countries – salt substitutes, community awareness, self-monitoring and combination pills - that could be scaled up in Australia with the potential to save millions of lives.
Professor Anushka Patel, Vice Principal Director & Chief Scientist, The George Institute for Global Health
Many subgroups of people with or at risk of cardiovascular diseases and diabetes have not benefitted from treatment advances, either because they have not been adequately tested in these groups, or because some are not receiving treatments already proven to be effective.
Projects will test if a ‘polypill’ can help women with or at risk of a certain type of heart failure, whether drug treatments for diabetes can prevent disease progression in women with recent gestational diabetes and expand the remit of The George Institute’s SMARThealth digital platform to help under-resourced health systems better manage a broader range of chronic conditions.
Simon Finfer, Professorial Fellow in the Critical Care Division at The George Institute for Global Health
Almost half of the 18,000 Australians treated for sepsis in ICUs each year die, and those who do survive have considerable long term health consequences, leading to annual treatment costs of over $1.5 billion.
As sepsis can result from any type of infection, people respond differently to treatment. Professor Finfer and his team will use existing research and new studies to better match the right treatment to the right patient, ultimately reducing death and disability from sepsis.
Polly Huang, Senior Data Analyst, The George Institute for Global Health
Globally, excess salt consumption (more than five grams per day) is responsible for three million deaths each year, with four out of five occurring in low- and middle-income countries, and nearly half among people younger than 70.
Dr Huang’s project will expand on The George Institute’s existing research to further build the case for wider adoption of salt substitutes – in which some of the sodium is replaced by potassium – which could prevent millions of deaths each year, particularly in low-income countries.
Jacqui Webster, Head of Advocacy and Policy Impact, The George Institute for Global Health
Unhealthy diets are now the leading cause of chronic disease around the world, driving catastrophic levels of obesity, cardiovascular disease, type 2 diabetes and some cancers, particularly in remote communities.
Professor Webster and her team will work across Australia and the Pacific Region to improve the food environment by making food policies more effective, improving food and water security, and reducing sodium in the food supply by encouraging adoption of the WHO Sodium Benchmarks and increasing the uptake of reduced sodium salts.
Jagnoor Jagnoor, Program Lead, Injury Program, The George Institute for Global Health
Globally 270,000 people die by drowning each year, mainly in low- and middle-income countries with the majority in the 1-10 year age group, and those living in rural areas. In high-income countries, ethnic minorities, migrants, and rural residents are over-represented.
This project aims to better understand the role of social disadvantage in drowning risk in order to design and implement more effective solutions and identify “best-buy” policies to reduce drowning deaths in the most affected communities.
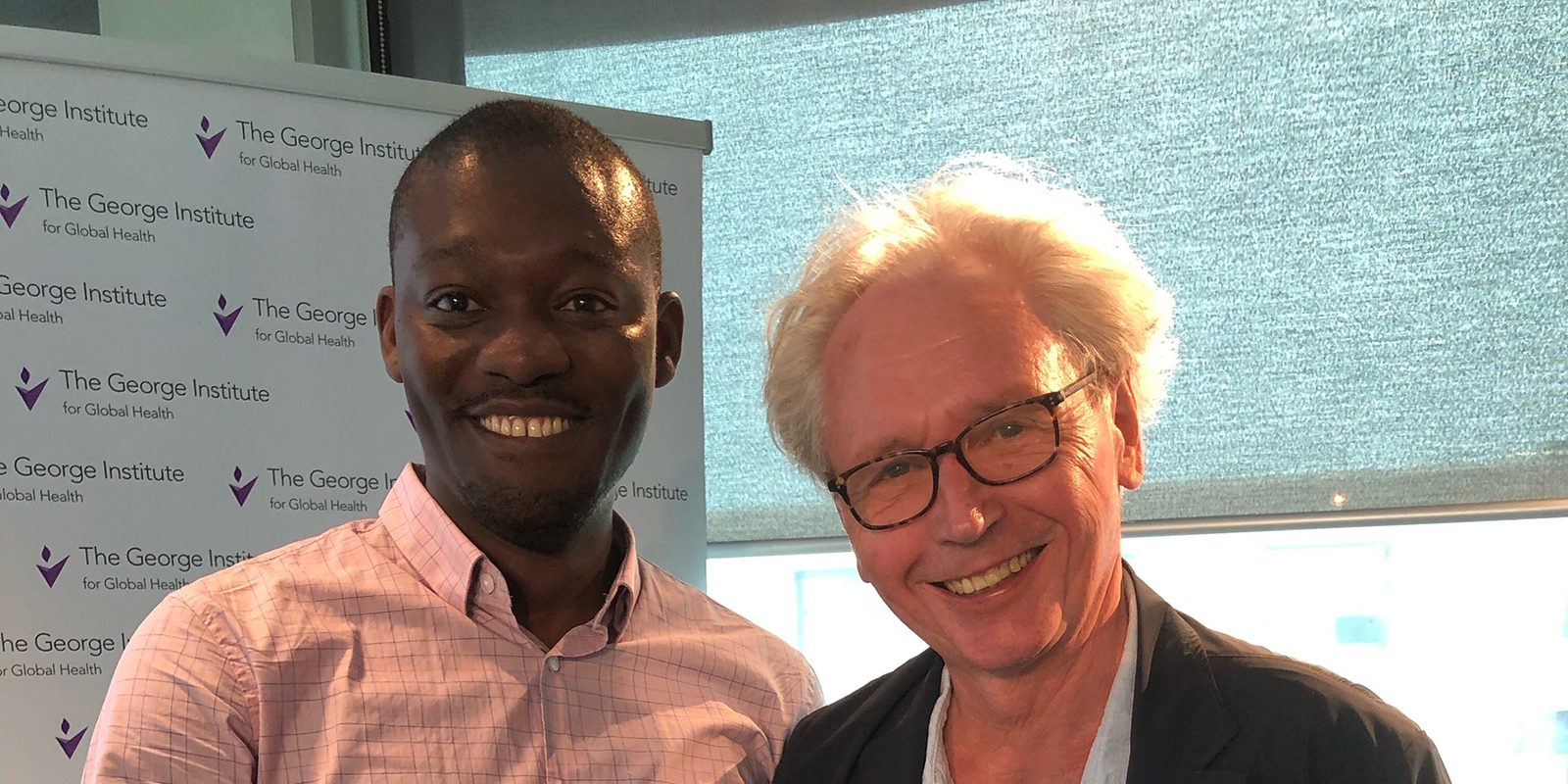
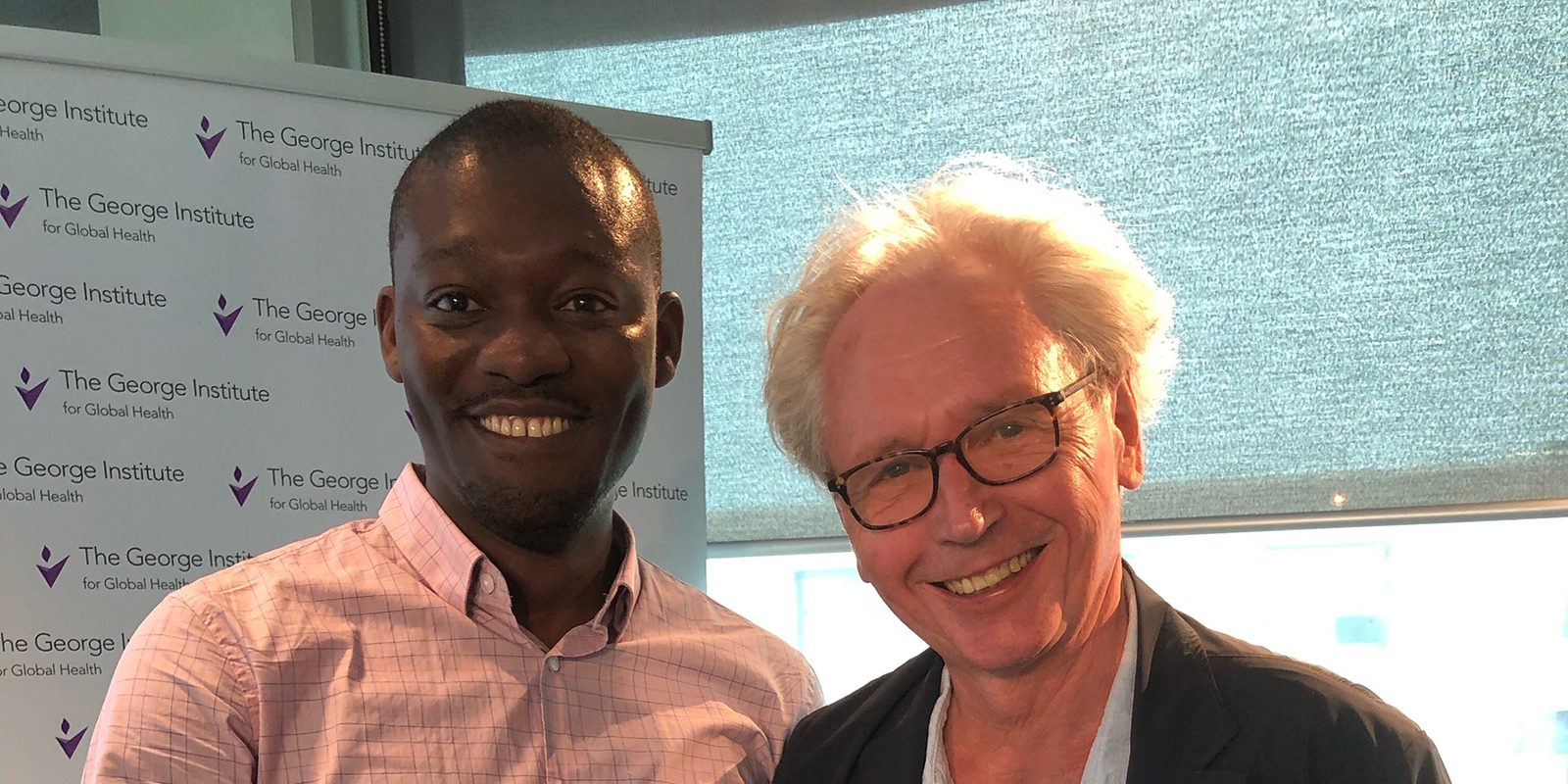
Bobby Porykali, Research Fellow, Guunu-maana (Heal) Aboriginal and Torres Strait Islander Health Program
Employment is a key social determinant of health - the longer someone is unemployed the greater their risk of suffering from a range of physical and mental health issues.
Building on previous findings that culturally appropriate driver licensing programs can increase Aboriginal and Torres Strait Islander peoples’ workforce participation, Dr Porykali’s project aims to connect such programs with self-determined pathways into employment, thereby improving health and wellbeing.