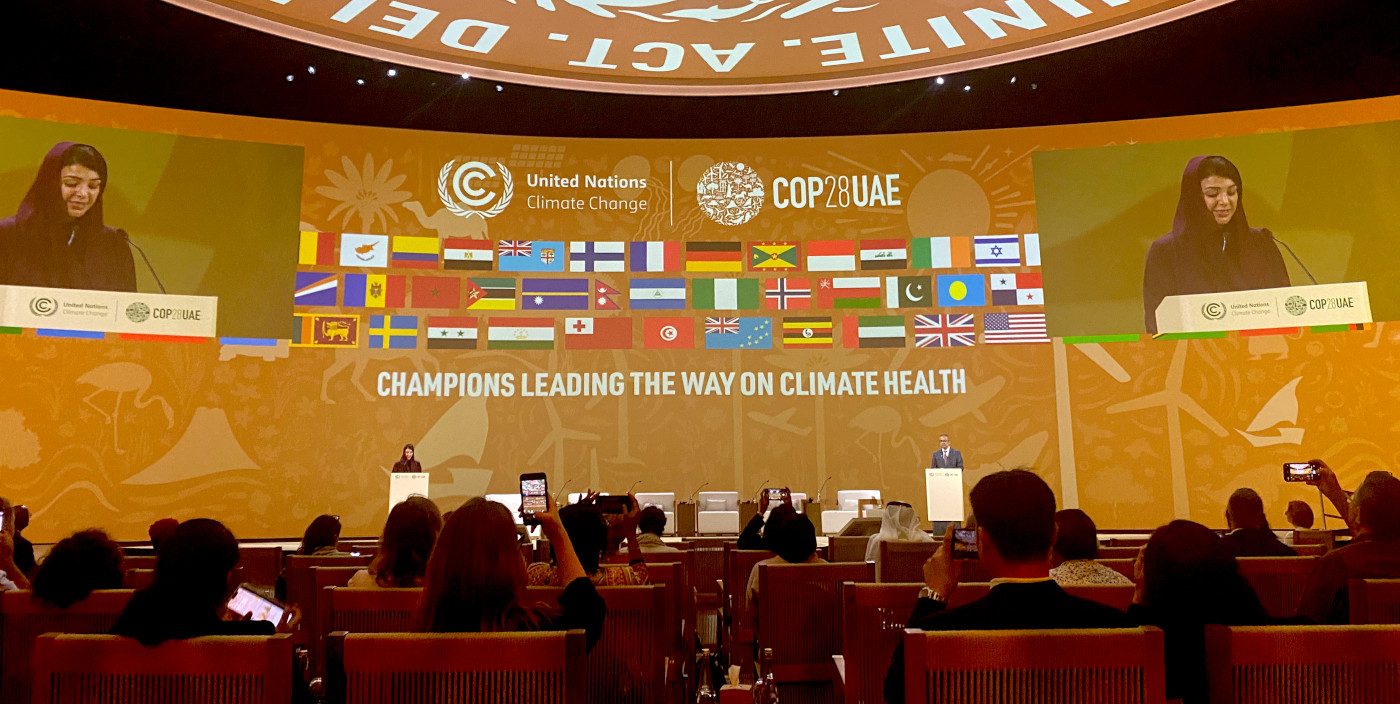
From November 30 to December 12, the Twenty-eighth session of the Conference of the Parties (COP28) in Dubai brought together leaders from around the world to discuss how to limit global temperature rises and adapt to the impacts of climate change. The George Institute for Global Health was among 1,900 health representatives, and called for leaders to centre the voices of communities whose health, well-being and futures have been most impacted, ensuring they are at the heart of national climate action plans and debate.
The inaugural Health Day was a significant milestone, spotlighting the critical connection between climate change and human health, a topic neglected in the past 28 years of COPs. Alongside this event, various high-level gatherings, a two-week World Health Organization (WHO) Health Pavilion, and health installations underscored the urgency of addressing the climate crisis to protect human lives. The engagement of over 50 health ministers in the Climate-Health Ministerial and endorsements from 140+ countries for the United Arab Emirates (UAE) Declaration on Climate and Health showed promise. Many delegates related stories of significant impacts on health arising from the impacts of global warming. The Director General of the WHO, Dr Tedros Adhanom Ghebreyesus, highlighted in several forums that more than 7 million people die every year due to air pollution from the burning of fossil fuels. It was noted that public health gains achieved in the 20th century are being reversed by climate change, with increased incidence of infectious diseases such as malaria and dengue fever of particular concern. While some delegates spoke about the interactions with non-communicable diseases and injuries (NCDIs), it was clear that more work needs to be done to highlight the implications of global heating in this area.
It’s imperative that the commitments made in the Declaration on Climate and Health are translated into action, ensuring sustained attention to Health Day in future COPs and mainstreaming health as pivotal for ambitious climate action in COP and other policy-making spaces, including the forthcoming World Health Assembly in 2024. Although the Declaration acknowledged the link between healthy populations and climate resilience across sectors like food, water, housing, and energy, overall COP28 outcomes fell short. Some high-income countries hesitated to recognise their primary responsibility in reducing emissions and failed to commit to financially support adaptation and mitigate loss and damage in the most impacted regions. One of the positive outcomes of Health Day was the collaborations that are emerging. For example, US $1 billion in funding was announced to kickstart implementation of the health declaration, with contributions from development banks, climate funds and large philanthropic organisations. The WHO in partnership with others has developed a set of financing principles for climate and health initiatives to help support implementation. While the funding is still small relative to the need, it indicates that there is an increasing understanding of the links between climate and health which can be built on in future. In addition, the Australian Government launched its first National Health and Climate Strategy, which highlights the importance of investing in research to improve the evidence base for responses to climate change. We hope to see this translate into funding for implementation.
Encouragingly, the UAE Declaration on Climate and Health emphasises the importance of strengthening health systems to anticipate and implement adaptation measures against climate-sensitive health risks (such as climate-health information services, surveillance, and early warning and response systems). However, we need a more robust emphasis on developing climate risk and vulnerability assessments for high-risk communities and leveraging digital platforms to generate high-quality data for decision-making. Strengthening primary health care services is also crucial, given their role as the primary point of access for many communities, and ability to provide essential mental health support—a critical response to the significant health impacts of the climate crisis.
COP28 celebrated key accomplishments, notably being termed the most 'Inclusive COP.' It introduced the People's Plenary, providing civil society with a formal platform to voice expectations. There were dedicated days focused on the experience of climate impacts by Indigenous peoples and women, and their respective roles in driving community-led climate action. The inclusion of diverse constituencies is a welcome development, but it was noted during discussions that there are still too few of these constituencies represented in the formal negotiations. The first Youth Stocktake offered a comprehensive analysis of youth involvement in climate diplomacy, serving as a blueprint for enhancing their participation in future COPs. Additionally, a $220 million funding package for Africa aimed at improving youth health and an upcoming dialogue in 2024 on the impacts of climate change on children and youth indicated progress in engaging communities in policymaking. These initiatives should set a precedent and be expanded to support other groups experiencing marginalisation, including Indigenous communities.
In contrast to previous conferences, COP28 also prioritised mostly plant-based catering and starting food emissions labelling on certain products, which is a positive development after concerns raised by Coca Cola’s sponsorship of COP27, also described as a “de-facto sponsor of the obesity epidemic causing diabetes and other NCDs”. Our innovative ecoSwitch app aims to support consumers in making healthy and more sustainable choices, using data on the greenhouse gas emissions associated with a product’s ingredients - a key driver of global heating– to assign a planetary health rating and suggest alternative products with a lower environmental impact. Yet notable increase in meat and dairy lobbyists, tripling compared to the previous year to a total of 340, alongside the continued substantial presence of at least 2,456 lobbyists from the fossil fuel industry, remains raises concerns about the potential for undue influence on the outcomes of COP.
The outcomes of the Global Stocktake rightly recognised the substantial contributions of various non-governmental stakeholders toward limiting global warming to 1.5°C. The George Institute in its new capacity as an Official Observer to the UN Framework Convention on Climate Change (UNFCCC) looks forward to engaging even more substantively with the COP in future. Through our emerging Planetary Health Initiative, we will continue to enhance knowledge on and address knowledge gaps in adaptation and availability of information on climate change impacts, including for monitoring and progress –.
Further information:
- Read Veronica Le Nevez' insights on the COP28 Outcome's inaugural global stocktake, accessible here.
- Explore the latest Health Policy Watch article titled ‘From Australia to Bangladesh and Beyond: Mobilizing Local Communities Is Key to Breaking Down Climate and Health Silos’, authored by Chhavi Bhandari, Emma Feeny, and Kez Bennett Brook.
- Discover The George Institute's COP priorities, including our Conference delegation.
- Explore our Planetary Health Brochure, summarising our initiatives and dedication to advancing evidence-informed action to improve planetary health.